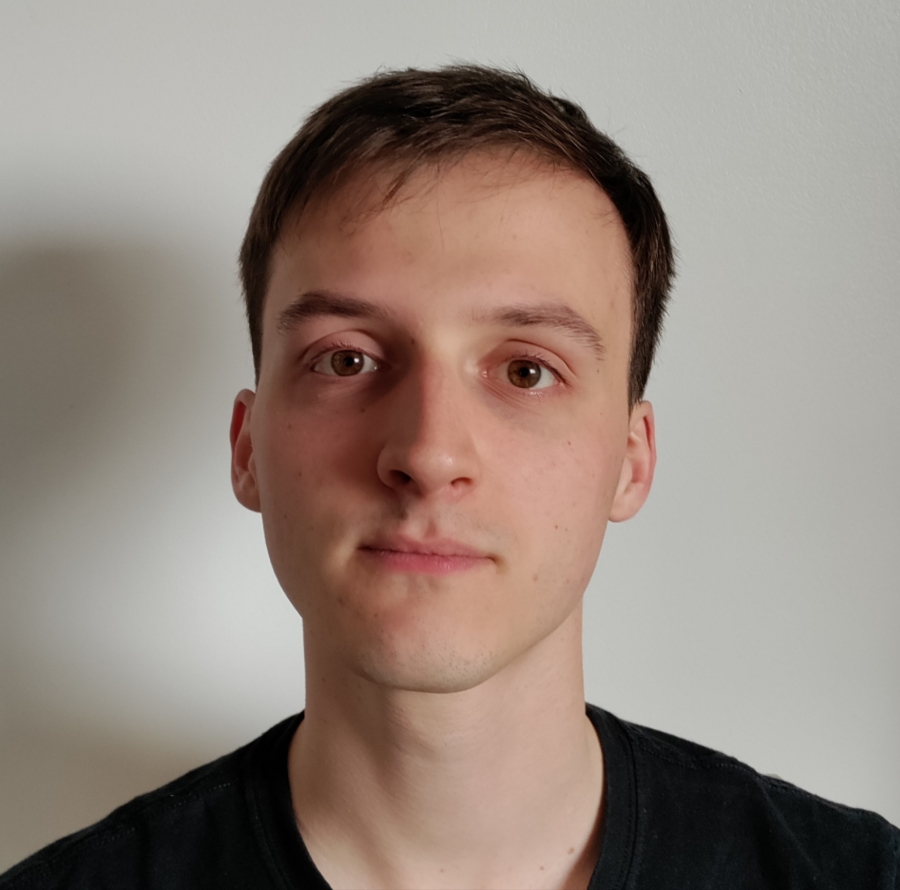
Hi, my name is Jake Walker. I work as a Psychological Wellbeing Practitioner (PWP) at NHS Talking Therapies Greater Preston.
Can you tell us a bit about the service you work in?
I work in the NHS Talking Therapies service. We provide psychological support for individuals who are struggling with common mental health problems including anxiety, depression, panic disorder, post-traumatic stress disorder (PTSD) and obsessive-compulsive disorder (OCD).
What does an average day look like for you as a psychological wellbeing practitioner?
An average day for a PWP can be pretty varied. Firstly, I start by preparing for my first appointment of the day, which is usually at 9.30am. While ongoing treatment sessions are brief, a course of 1 to 1 guided self-help with a PWP can drastically improve a person’s quality of life, and help them develop a foundation of coping strategies to manage their own mental health into the future. I also complete telephone triage assessments for individuals referring into the service, to help allocate them the best support for their needs.
Every Friday, I co-facilitate the wellbeing workshop, which is a weekly group psycho-educational course. Our team also has ‘champion’ roles, which allow practitioners to work around one area of practice; I am one of two veterans champions in our service, so we meet regularly to work on making the service more accessible for military veterans. The role of PWP is very flexible in allowing you to take on these kind of additional responsibilities, depending on what suits your strengths as a practitioner.
I might end the day with attending caseload management, which comprises a weekly 1 to 1 supervision session with a senior PWP in the service. I primarily discuss the patients on my caseload, but supervision also gives you a chance to decompress and talk about the working week! I think having this time is very important and helps avoid feelings of burnout or depletion.
In your experience what impact can psychological wellbeing practitioners have on delivering high quality health care?
Psychological wellbeing practitioners have an extremely important role in the psychological professions. Having access to early and timely intervention is critical to prevent a service user’s mental needs from escalating. This preventative approach also helps to relieve pressure on specialist and secondary care services within the NHS.
From the initial discussion about treatment goals, through to the service user’s eventual discharge, we always aim to ensure that the patient has a say in the decisions regarding their care. Mental health care in the NHS can be intimidating to navigate, therefore it’s greatly important that the service user is informed and involved in their care. Failing to ensure this may cause the service user to disengage from services and return when their needs have escalated and they require more intensive support.