Introduction
The way you eat is an important part in the treatment of gestational diabetes. The food you eat needs to provide suitable nourishment for both you and your baby, whilst helping to stabilise your blood glucose levels.
This leaflet will give you information to get started.
In the Joint Diabetes and Antenatal Clinic you will have the opportunity to discuss the food you eat with a registered dietitian.
You will be given individual advice to help manage your Gestational Diabetes. In addition to this it is important to remember the following:
- Watch portion sizes.
- Try to choose options that are lower in fat, salt and sugar when you can.
- Limit intake of high fat foods and high calorie snacks e.g. crisps, cakes, biscuits to prevent too much weight gain.
- Get your 5 portions of fruit and vegetables a day.
Eight Steps To Manage Blood Glucose Levels
1. Eat less sugary carbohydrate
2. Reduce portion sizes of starchy carbohydrate.
3. Spread carbohydrate out throughout the day.
4. Try not to miss meals.
5. Have regular snacks
6. Have a starchy supper.
7. Choose starchy carbohydrates that break down more slowly (Low G.I.)
8. Be more active.
Carbohydrates Carbohydrate foods are the best energy sources for your body. When they are digested, they break down to form glucose in the bloodstream.
Carbohydrate is the only food group that directly affects blood glucose levels.
Where are carbohydrates found?
Sugar and sugary foods
Sweets, chocolates, sweetened drinks, fruit juice, cakes, biscuits, Indian sweets.
The glucose in these foods is quickly absorbed into the bloodstream making blood glucose levels rise quickly.
Starchy foods
Bread, potatoes, rice, pasta, noodles, chapatti, breakfast cereals, yam, crisps, fufu, gari, swallow, plantain.
After digestion, these foods are slowly absorbed into the bloodstream making blood glucose levels rise more slowly.
Milk and fruits
Milk, yoghurt and fruit all contain natural sugars which will cause blood glucose levels to rise.
Sugary Carbohydrates
A healthy eating plan for gestational diabetes can include some sugar e.g. foods such as sweet biscuits, jam and honey can be eaten in small amounts. Having sugary foods and drinks in large amounts, or regularly, will affect your blood glucose readings. The amount of sugary food you eat or drink will affect how high your blood glucose levels rise.
- Avoid sugary drinks - energy drinks, fizzy pop, pure fruit juice and smoothies.
- Avoid adding sugar to hot drinks or to food.
- Avoid sugar coated or chocolate cereals.
- There is no need for any special foods when you have diabetes.
- Diabetic foods are not recommended.
| Instead of these: | Use these: |
| Sugar, glucose powder, honey, gur, jaggery | Artificial sweeteners e.g Canderel, Hermasetas, Splenda |
| Sugar and chocolate coated cereals, sweetened muesli | Weetabix, Shredded Wheat, porridge, bran flakes, unsweetened muesli |
| Ordinary jam, marmalade, honey, syrup, lemon curd, treacle, molasses, sweet sauces e.g sweet chilli, sweet and sour | Nut butters e.g peanut butter, Marmite/Vegemite |
| Cakes, pastries, chocolate and cream-filled biscuits | Plain scones, muffins, crumpets, currant/fruit buns, plain biscuits e.g digestive, rich tea, morning coffee. |
| Tinned fruit in syrup | Fresh fruit |
| Sweetened puddings e.g rice pudding, custard, instant whips and mousses, flavoured ice cream | No added sugar rice puddings and custard. Sufar free jellies, instant whips and mousses. Plain ice cream. |
| Sweets, chocolates, mints, fudge, toffee, indian sweets | Small amounts of sugar free mints and chewing gum |
| Ordinary squash and fizzy drinks, e.g Ribena, lemonade, Lucozade, cola, smoothies and milkshakes | Sugar free and diet drinks, low calorie hot chocolate with sweetener. |
Starchy Carbohydrates and Portion Control
Regular meals spread throughout the day will help to maintain your energy levels without causing big rises in your blood glucose levels.
The amount of starchy carbohydrate you eat will affect how high your blood glucose level rises after a meal.
Choose just one source of starchy carbohydrate with each meal. E.g. Avoid meals such as lasagne and chips, curry with chapatti and rice, pasta and garlic bread.
Some meals consist of mostly carbohydrate, e.g. pizza, pasta, risotto, biryani / biriani. Have these in small amounts and fill up with salad/ vegetables.

Glycaemic Index (G.I)
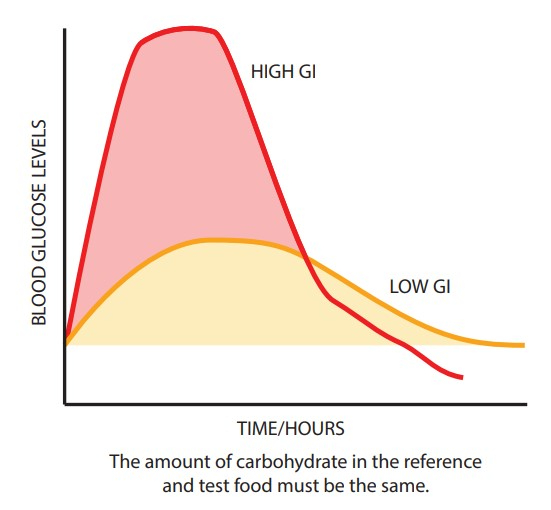
The type of starchy carbohydrate foods you choose can have an effect on your blood glucose levels.
Choosing slow release , low G.I., foods may slow down the rise in your blood glucose levels after a meal.
You can slow down glucose levels by adding protein to meals e.g. greek yoghurt with fruit, nut butter to seeded bread and dressing on salad.
Some Low G.I. carbohydrate choices.
| Carbohydrate food | Lower G.I choice |
| Bread (white bread and rolls) | Multigrain, granary, rye, seeded, wholegrain, oat, pitta bread, chapatti made with wholemeal flour. |
| Potatoes (mashed) | New potatoes in their skins, small baked potatoes, sweet potato and yam |
| Pasta | All pasta cook until el dente. Noodles, look for wholemeal choices. |
| Rice (white) | Basmati rice, long grain and brown rice. |
| Other grains | Bulgur wheat, barley, cous cous and quinoa. |
| Breakfast cereals (cornflakes, rice krispies, chocolate, sugar coated) | Porridge, most oat and brain based cereals. Small portions. |
Impact of food on blood sugar
Snacking
- It is important not to have large gaps between meals.
- Try to spread out your food each day and have a small snack or your meal every two hours.
- Fruit is a healthy snack. Spread it out throughout the day. Have no more than one palm sized portion at a time.
- Avoid having milky drinks with meals and snacks e.g. milk shakes, smoothies, lattes, cappuccinos.
- Instead, have them on their own as a snack.
- If you have a sandwich for lunch save any extras such as yoghurts, crisps, fruit to use as snacks throughout the day. Try to have a snack before going to bed e.g. toast / cereal.
Snack Ideas
- Two oatcakes with cream cheese.
- Two crackers / crisp breads with cheese.
- Two multigrain crispbreads with hummus.
- Salted or unsweetened popcorn.
- One slice of peanut butter on toast.
- One standard sized packet of crisps.
- One piece of fruit.
- Three breadsticks and salsa / sour cream and chive, hummus, tzatziki, raita dip.
- Two plain biscuits e.g. rich tea, digestive biscuits.
- Standard sized pot of yoghurt.
- Snack box of raisins.
- Palm sized portion of fruit e.g. one apple, one orange, two plums, 12 grapes, small slice of mango or melon.
- Two small samosas or pakoras.
- One handful bombay mix / chevra.
- Two idli.
- One small roti / paratha
- Nutty cereal bars
- Sugar free jelly
- Handful of nuts
Suggested Meal Ideas Breakfast
- Porridge and milk.
- Greek yoghurt/skyr with berry, fruits and oats.
- Hard boiled or poached egg and wholegrain toast.
- Reduced sugar baked beans and one slice of toast.
- Small bowl wholegrain/multi-grain cereal and milk (e.g. Cheerios / branflakes, Shredded Wheat).
- Bacon sandwich - one slice of bread.
- Cheese on toast - one slice.
- Bacon, egg, tomatoes, mushrooms, beans and one slice of toast.
- Small roti/chappati with vegetable curry Lunch
Lunch
- Sandwich (two slices of bread or small barm or roll) with salad.
- Small jacket potato and tuna, cheese or cottage cheese.
- Bowl of soup and small bread roll.
- Meat / fish / egg curry with one medium chapatti.
- Lentil curry with salad and half a chapatti.
- One wrap with meat, fish or cheese filling and salad.
Evening Meal
- Small bowl of pasta with salad.
- Roast meat/chicken, two to three potatoes, and lots of vegetables.
- Chilli con carne and one third of a plate of rice with salad.
- Meat/chicken/fish or Quorn Stir fry with a small bowl of noodles.
- Two slices of pizza and salad.
- Meat kebab, salad, and small pitta bread.
- Small bowl of biriyani and salad.
- Cooked salmon, new potatoes and vegetables.
- Chicken, vegetables and smaller portion of plantan, sweetpotatoes, fufu, swallow or gari.
Action plan
Try to pick three things to try and achieve before you go to the joint diabetes and antenatal clinic.
Tried
- Start having breakfast
- Have smaller portions at mealtimes
- Have more fruit and vegetables
- Use 'diet' or 'no added sugar' drinks
- Have snacks between meals
- Be more active
- Stop skipping meals
- Include a supper bedtime
Changed
- Start having breakfast
- Have smaller portions at mealtimes
- Have more fruit and vegetables
- Use 'diet' or 'no added sugar' drinks
- Have snacks between meals
- Be more active
- Stop skipping meals
- Include a supper bedtime
